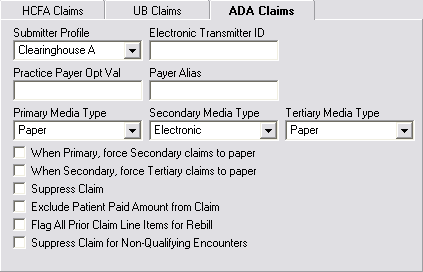
| Submitter Profile | Select the submitter profile that you want to apply to ADA claims. |
|---|
| Electronic Transmitter ID | Enter the payer-assigned electronic transmitter ID to generate a claim with an electronic transmitter ID.
Note: This field only displays when you select a submitter profile.
|
|---|
| Practice Payer Opt Val | Enter the practice/payer-specific value. |
|---|
| Payer Alias | Enter an alternative payer name when a name that differs from the name that appears in the payer's Payer master file is required. |
|---|
| Primary, Secondary, and Tertiary Media Types | Enter the primary media type accepted by the clearinghouse as being electronic or paper. If you set it as electronic, then you can also set how the secondary and tertiary claims should be submitted. |
|---|
| When Primary, force Secondary claims to paper | Select this check box if you want the claim being sent to the secondary insurance to be generated on paper after payment from the primary insurance has been received. This action overrides the Electronic Secondary Media Type setting. |
|---|
| When Secondary, force Tertiary claims to paper | Select this check box if you want the claim being sent to the tertiary insurance to be generated on paper after payment from the primary and secondary insurances have been received. This action overrides the Electronic Tertiary Media Type setting. |
|---|
| Suppress Claim | Check this box to suppress claims by payer when creating claims in batch mode only. |
|---|
| Exclude Patient Paid Amount from Claim | Select this check box to suppress patient paid amounts from UB EDI files. Segment AMT*F5 is not present in the EDI file.
Note: When the check box is not selected, the amount is not suppressed and segment AMT*F5 is present in the EDI file.
|
|---|
| Flag All Prior Claim Line Items for Rebill | Select this option to include line items with a $0.00 amount with the other line item charges when you rebill an archived claim. |
|---|
| Suppress Claim for Non-Qualifying Encounter | Select this check box to suppress claims for this payer when creating claims for non-qualifying encounters to a federally qualified health center. |
|---|