Claim Edits Library for Behavioral Health Billing
Two claim edits are available that may be enabled and set up for Behavioral Health billing, though they may also be used for non-behavioral health billing purposes. Each edit is configurable with specific CPT4 codes.
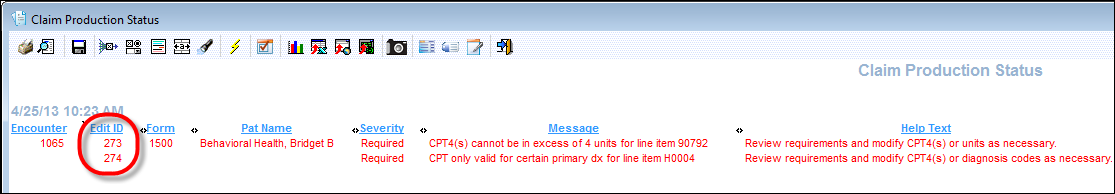
- 273 CPT4(s) cannot be in excess of a particular number of units
Select this edit if specific CPT4 codes cannot exceed a specified number of units during charge posting.
- 274 CPT4(s) only valid for certain primary dx
Select this edit if specific CPT4 codes can only be used with specified primary ICD codes during charge posting.
Example: When billing a state behavioral health program (payer) for a drug and alcohol abuse CPT4, the primary ICD code must be drug or alcohol related.
The claim edits fail when a charge for a specified CPT4 code exceeds the defined number of units (#273), or a charge for a specified CPT4 code does not have one of the defined ICD codes as the primary diagnosis (#274).